Electronic Data Interchange(EDI):
What
is EDI??
Business
processes in a large variety of industries are becoming increasingly digitized.
In the new era of the paperless office, it is not uncommon for all kinds of
data to be transferred electronically rather than on paper. The healthcare
industry is no exception, and electronic attachments for insurance claims are
just one type of EDI in healthcare. But what is EDI? Electronic data
interchange is more than just email; it is a structured way to transmit data
between computer systems, governed by standards that are extremely important
for medical claims.
Organizing and sending data between parties in
the medical and dental industries has always been a complicated process,
particularly in the management of both patient medical records and health
insurance reimbursement details. However, thanks to increases in efficiency,
EDI implementation has proven to both save time and save money. An important
element in EDI is that of standards. Each EDI document has a standardized
format, which ensures that data can be quickly sent and interpreted on both
sides. It is particularly important that providers and payers utilizing
healthcare EDI transactions follow HIPAA regulations and ANSI standards. EDI
formatting specifications are like blueprints for data, EDI guides that serve
to make transitions between different data trading partners as smooth as
possible.
The reason
that EDI has become especially important with respect to insurance claim
documentation is the proven increase in efficiency seen with the use of
electronic attachments. Not only do electronic attachments streamline the
process, but CMS and commercial payers also require medical necessity
documentation for certain procedures or events. When supporting documentation
is included along with an initial electronic claims submission, both providers
and payers can see the benefits, such as fewer denials and rework requests and
an increase in ROI. In fact, even though attachments only represent a small
part of the electronic claims process (perhaps 10% of claims); they have been
shown to have a significant impact on the speed of insurance reimbursement.
Why
EDI??
• A
Decades-Old Quest
– 1950s First Steps
– 1960s Tape-based
standards
– 1970s
Industry-Specific Standards
– 1980
Cross-Industry Standards
– 1990s EDI evolves
into EC
– 2000s Stay Tuned!
• Electronic
Data Interchange:
– The exchange of
computer-processable data in a
standardized format between two enterprises.
• Electronic
Commerce:
– Any use of a variety of
technologies that eliminate
paper and substitute electronic alternatives for data collection and exchange.
Options include Interactive Voice Response, Fax, Email, Imaging, Swipe Cards
and multiple Web-based Internet tools.
EDI
and EC: A Place for Both
• EDI
– Standards-based data exchange - the
foundation of quality transaction processing.
– System to system exchanges of highly structured
data.
– HIPAA
MANDATES EDI STANDARDS!
• Electronic
Commerce:
– Multiple ways to
communicate unstructured data.
– People-to-system
or people-to-people exchanges.
What Standards?
• What is ANSI?
– American National Standards Institute
– Since 1917 the only source of American
National
Standards
•
What is ASC X12
– Accredited Standards Committee X12, chartered
in
1979
– Responsible for cross-industry standards for electronic documents
EDI
Standards = Paper Forms
Paper records use forms to organize information. EDI uses standard transaction sets.
Healthcare Claim =
837
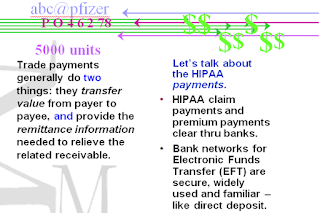
Payment &
Remittance = 835
Invoice = 810
Purchase Order =
850
Converting standard forms into standard messages …
Standard Forms and
Standard Formats
Which
means strings of text …Called Segments
Segment ID Segment Terminator
Segment
Delimiter
… Composed
of smaller pieces...
(Segments are composed of
“data elements.”)
Individual Name Last Name Middle Initial
NM1*P2*1*Clinton*Hilary*R~
Insured Person First Name
The
standards are meant to improve the efficiency and effectiveness of the American
health care system by encouraging the widespread use of EDI in the U.S health
care system. The HIPAA EDI transaction sets are based on X12 and the key
message types are described below:
EDI Benefit Enrollment and Maintenance Set (834)
Can be used
by employers, unions, government agencies, associations or insurance agencies
to enroll members to a payer. The payer is a healthcare organization that pays
claims, administers insurance or benefit or product. Examples of payers include
an insurance company, health care professional (HMO), preferred provider organization
(PPO), government agency (Medicaid, Medicare etc.) or any organization that may
be contracted by one of these former groups.
EDI Health Care Claim Transaction set (837)
Used to submit
health care claim billing information, encounter information, or both, except
for retail pharmacy claims (see EDI Retail Pharmacy Claim Transaction). It can
be sent from providers of health care services to payers, either directly or
via intermediary billers and claims clearinghouses. It can also be used to
transmit health care claims and billing payment information between payers with
different payment responsibilities where coordination of benefits is required
or between payers and regulatory agencies to monitor the rendering, billing,
and/or payment of health care services within a specific health care/insurance
industry segment.
For example,
a state mental health agency may mandate all healthcare claims, Providers and
health plans who trade professional (medical) health care claims electronically
must use the 837 Health Care Claim: Professional standard to send in claims. As
there are many different business applications for the Health Care claim, there
can be slight derivations to cover off claims involving unique claims such as
for Institutions, Professionals, Chiropractors, and Dentists etc.
EDI Health Care Claim Payment/Advice Transaction Set (835)
Can be used to make a payment, send an Explanation of
Benefits (EOB) remittance advice, or make a
payment and send an EOB remittance advice only from a health insurer to a
health care provider either directly or via a financial institution.
EDI Payroll Deducted and other group Premium Payment for
Insurance Products (820)
A
transaction set which can be used to make a premium payment for insurance
products. It can be used to order a financial institution to make a payment to
a payee.
EDI Retail Pharmacy Claim Transaction (NCPDP Telecommunications Standard version 5.1)
Used to
submit retail pharmacy claims to payers by health care professionals who
dispense medications, either directly or via intermediary billers and claims
clearinghouses. It can also be used to transmit claims for retail pharmacy
services and billing payment information between payers with different payment
responsibilities where coordination of benefits is required or between payers and
regulatory agencies to monitor the rendering, billing, and/or payment of retail
pharmacy services within the pharmacy health care/insurance industry segment.
EDI Health Care Eligibility/Benefit Inquiry (270)
Used to
inquire about the health care benefits and eligibility associated with a
subscriber or dependent.
EDI Health Care Eligibility/Benefit Response (271)
Used to
respond to a request inquire about the health care benefits and eligibility
associated with a subscriber or dependent.
EDI Health Care Claim Status Request (276)
This
transaction set can be used by a provider, recipient of health care products or
services or their authorized agent to request the status of a health care
claim.
EDI Health Care Claim Status Notification (277)
This
transaction set can be used by a health care payer or authorized agent to
notify a provider, recipient or authorized agent regarding the status of a
health care claim or encounter, or to request additional information from the
provider regarding a health care claim or encounter. This transaction set is
not intended to replace the Health Care Claim Payment/Advice Transaction Set
(835) and therefore, is not used for account payment posting. The notification
is at a summary or service line detail level. The notification may be solicited
or unsolicited.
EDI Health Care Service Review Information (278)
This
transaction set can be used to transmit health care service information, such
as subscriber, patient, demographic, diagnosis or treatment data for the
purpose of request for review, certification, notification or reporting the
outcome of a health care services review.
EDI Functional Acknowledgement Transaction Set (997)
2. 837 EDI Claims
EDI 837 Health Care Claim:
The EDI 837 transaction set is the format
established to meet HIPAA requirements for the electronic submission of
healthcare claim information. The claim information included amounts to the
following, for a single care encounter between patient and provider:
§ A description of the patient
§ The patient’s condition for which
treatment was provided
§ The services provided
§ The cost of the treatment
As of March 31,
2012, healthcare providers must be compliant with version 5010 of the HIPAA EDI
standards. The 5010 standards divide the 837 transaction set into three groups,
as follows: 837P for professionals, 837I for institutions and 837D for dental
practices. The 837 is no longer used by retail pharmacies.
This transaction set is sent by the providers to payers, which include insurance companies, health maintenance organizations (HMOs), preferred provider organizations (PPOs), or government agencies such as Medicare, Medicaid, etc. These transactions may be sent either directly or indirectly via clearinghouses. Health insurers and other payers send their payments and coordination of benefits information back to providers via the EDI 835 transaction set.
This transaction set is sent by the providers to payers, which include insurance companies, health maintenance organizations (HMOs), preferred provider organizations (PPOs), or government agencies such as Medicare, Medicaid, etc. These transactions may be sent either directly or indirectly via clearinghouses. Health insurers and other payers send their payments and coordination of benefits information back to providers via the EDI 835 transaction set.
EDI 837 Format:
ISA*00* *00* *ZZ*99999999999 *ZZ*888888888888 *111219*1340*^*00501*000001377*0*T*>
GS*HC*99999999999*888888888888*20111219*1340*1377*X*005010X222
ST*837*0001*005010X222
BHT*0019*00*565743*20110523*154959*CH
NM1*41*2*SAMPLE INC*****46*496103
PER*IC*EDI DEPT*EM*FEEDBACK@1EDISOURCE.COM*TE*3305551212
NM1*40*2*PPO BLUE*****46*54771
HL*1**20*1
PRV*BI*PXC*333600000X
NM1*85*2*EDI SPECIALTY SAMPLE*****XX*123456789
N3*1212 DEPOT DRIVE
N4*CHICAGO*IL*606930159
REF*EI*300123456
HL*2*1*22*1
SBR*P********BL
NM1*IL*1*CUSTOMER*KAREN****MI*YYX123456789
N3*228 PINEAPPLE CIRCLE
N4*CORA*PA*15108
DMG*D8*19630625*M
NM1*PR*2*PPO BLUE*****PI*54771
N3*PO BOX 12345
N4*CAMP HILL*PA*17089
HL*3*2*23*0
PAT*19
NM1*QC*1*CUSTOMER*COLE
N3*228 PINEAPPLE CIRCLE
N4*CORA*PA*15108
DMG*D8*19940921*M
CLM*945405*5332.54***12>B>1*Y*A*Y*Y*P
HI*BK>2533
LX*1
SV1*HC>J2941*5332.54*UN*84***1
DTP*472*RD8*20110511-20110511
REF*6R*1099999731
NTE*ADD*GENERIC 12MG CARTRIDGE
LIN**N4*00013264681
CTP****7*UN
NM1*DK*1*PATIENT*DEBORAH****XX*12345679030
N3*123 MAIN ST*APT B
N4*PITTSBURGH*PA*152181871
SE*39*0001
GE*1*1377
IEA*1*000001377
GS*HC*99999999999*888888888888*20111219*1340*1377*X*005010X222
ST*837*0001*005010X222
BHT*0019*00*565743*20110523*154959*CH
NM1*41*2*SAMPLE INC*****46*496103
PER*IC*EDI DEPT*EM*FEEDBACK@1EDISOURCE.COM*TE*3305551212
NM1*40*2*PPO BLUE*****46*54771
HL*1**20*1
PRV*BI*PXC*333600000X
NM1*85*2*EDI SPECIALTY SAMPLE*****XX*123456789
N3*1212 DEPOT DRIVE
N4*CHICAGO*IL*606930159
REF*EI*300123456
HL*2*1*22*1
SBR*P********BL
NM1*IL*1*CUSTOMER*KAREN****MI*YYX123456789
N3*228 PINEAPPLE CIRCLE
N4*CORA*PA*15108
DMG*D8*19630625*M
NM1*PR*2*PPO BLUE*****PI*54771
N3*PO BOX 12345
N4*CAMP HILL*PA*17089
HL*3*2*23*0
PAT*19
NM1*QC*1*CUSTOMER*COLE
N3*228 PINEAPPLE CIRCLE
N4*CORA*PA*15108
DMG*D8*19940921*M
CLM*945405*5332.54***12>B>1*Y*A*Y*Y*P
HI*BK>2533
LX*1
SV1*HC>J2941*5332.54*UN*84***1
DTP*472*RD8*20110511-20110511
REF*6R*1099999731
NTE*ADD*GENERIC 12MG CARTRIDGE
LIN**N4*00013264681
CTP****7*UN
NM1*DK*1*PATIENT*DEBORAH****XX*12345679030
N3*123 MAIN ST*APT B
N4*PITTSBURGH*PA*152181871
SE*39*0001
GE*1*1377
IEA*1*000001377
EDI 837 Specification:
This X12 Transaction Set contains
the format and establishes the data contents of the Health Care Claim
Transaction Set (837) for use within the context of an Electronic Data
Interchange (EDI) environment. This transaction set can be used to submit
health care claim billing information, encounter information, or both, from
providers of health care services to payers, either directly or via intermediary
billers and claims clearinghouses. It can also be used to transmit health care
claims and billing payment information between payers with different payment
responsibilities where coordination of benefits is required or between payers
and regulatory agencies to monitor the rendering, billing, and/or payment of
health care services within a specific health care/insurance industry segment.
For purposes of this standard, providers of health care products or services
may include entities such as physicians, hospitals and other medical facilities
or suppliers, dentists, and pharmacies, and entities providing medical
information to meet regulatory requirements. The payer refers to a third party
entity that pays claims or administers the insurance product or benefit or
both. For example, a payer may be an insurance company, health maintenance
organization (HMO), preferred provider organization (PPO), government agency
(Medicare, Medicaid, Civilian Health and Medical Program of the Uniformed
Services (CHAMPUS), etc.) or an entity such as a third party administrator
(TPA) or third party organization (TPO) that may be contracted by one of those
groups. A regulatory agency is an entity responsible, by law or rule, for
administering and monitoring a statutory benefits program or a specific health
care/insurance industry segment.
3. 835 Remittance
EDI 835 Health Care Claim
Payment/Advice:
| The Electronic Remittance Advice (ERA), or 835,
is the electronic transaction which provides claim payment information in the
HIPAA mandated ACSX12 005010X221A1 format. These files are used by practices,
facilities, and billing companies to autopost claim payments into their
systems. You can receive your 835 files through your clearinghouse, direct
connection, or Connectivity Director, with enrollment in Electronic Payments
& Statements (EPS). Benefits:
· Eliminate
manual keying; save time and effort
· Reduce
posting errors
· Increase
efficiency and save money
|
EDI 835(Electronic Remittance Advice)
The EDI 835 transaction set is called Health Care
Claim Payment and Remittance Advice. It has been specified by HIPAA 5010
requirements for the electronic transmission of healthcare payment and benefit
information.
The 835 is used primarily by Healthcare insurance plans to make payments to healthcare providers, to provide Explanations of Benefits (EOBs), or both. When a healthcare service provider submits an 837 Health Care Claim, the insurance plan uses the 835 to detail the payment to that claim, including:
The 835 is used primarily by Healthcare insurance plans to make payments to healthcare providers, to provide Explanations of Benefits (EOBs), or both. When a healthcare service provider submits an 837 Health Care Claim, the insurance plan uses the 835 to detail the payment to that claim, including:
§ What charges
were paid, reduced or denied
§ Whether there
was a deductible, co-insurance, co-pay, etc.
§ Any bundling or
splitting of claims or line items
§ How the payment
was made, such as through a clearinghouse
A
particular 835 document may not necessarily match up one-for-one with a
specific 837. In fact, it is not uncommon for multiple 835 transactions to be
used in response to a single 837, or for one 835 to address multiple 837
submissions. As a result, the 835 is important to healthcare providers, to
track what payments were received for services they provided and billed.
EDI 835 Format:
ISA*00* *00* *ZZ*ABCCOM *ZZ*99999999 *040315*1005*U*00401*004075123*0*P*:
GS*HP*ABCCOM*01017*20110315*1005*1*X*004010X091A1
ST*835*07504123
BPR*H*5.75*C*NON************20110315
TRN*1*A04B001017.07504*1346000128
DTM*405*20110308
N1*PR*ASHTABULA COUNTY ADAMH BD*XX*6457839886
N3*4817 STATE ROAD SUITE 203
N4*ASHTABULA*OH*44004
N1*PE*LAKE AREA RECOVERY CENTER *FI*346608640
N3*2801 C. COURT
N4*ASHTABULA*OH*44004
REF*PQ*1017
LX*1
CLP*444444*1*56.70*56.52*0*MC*0000000655555555*53
NM1*QC*1*FUDD*ELMER*S***MI*1333333
NM1*82*2*WECOVERWY SVCS*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.70*56.52**6
DTM*472*20110205
CAS*CO*42*0.18*0
REF*6R*444444
CLP*999999*4*25.95*0*25.95*13*0000000555555555*11
NM1*QC*1*SAM*YOSEMITE*A***MI*3333333
NM1*82*2*ACME AGENCY*****FI*310626223
REF*F8*H57B10401
SVC*ZZ:M2200:HE*25.95*0**1
DTM*472*20021224
CAS*CR*18*25.95*0
CAS*CO*42*0*0
REF*6R*999999
CLP*888888*4*162.13*0*162.13*MC*0000000456789123*11
NM1*QC*1*SQUAREPANTS*BOB* ***MI*2222222
NM1*82*2*BIKINI AGENCY*****FI*310626223
REF*F8*H57B10401
SVC*ZZ:M151000:F0*162.13*0**1.9
DTM*472*20020920
CAS*CO*29*162.13*0*42*0*0
REF*6R*888888
CLP*111111*2*56.52*18.88*0*13*0000000644444444*53
NM1*QC*1*LEGHORN*FOGHORN*P***MI*7777777
NM1*82*2*CHICKENHAWK SVCS*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.52*18.88**6
DTM*472*20031209
CAS*CO*42*0*0
CAS*OA*23*37.64*0
REF*6R*111111
CLP*121212*4*56.52*0*0*13*0000000646464640*53
NM1*QC*1*EXPLORER*DORA****MI*1717171
NM1*82*2*SWIPER AGENCY*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.52*0**6
DTM*472*20031202
CAS*CO*42*0*0
CAS*OA*23*57.6*0*23*-1.08*0
REF*6R*121212
CLP*333333*1*74.61*59.69*14.92*13*0000000688888888*55
NM1*QC*1*BEAR*YOGI* ***MI*2222222
NM1*82*2*JELLYSTONE SVCS*****FI*346608640
REF*F8*A76B04054
SVC*ZZ:A0230:HF*74.61*59.69**1
DTM*472*20110203
CAS*PR*2*14.92*0
CAS*CO*42*0*0
REF*6R*333333
CLP*777777*25*136.9*0*0*13*0000000622222222*53
NM1*QC*1*BIRD*TWEETY*M***MI*4444444
NM1*82*2*GRANNY AGENCY*****FI*340716747
REF*F8*A76B03293
SVC*HC:H0015:HF:99:H9*136.9*0**1
DTM*472*20030911
CAS*PI*104*136.72*0
CAS*CO*42*0.18*0
REF*6R*777777
CLP*123456*22*-42.58*-42.58*0*13*0000000657575757*11
NM1*QC*1*SIMPSON*HOMER* ***MI*8787888
NM1*82*2*DOH GROUP*****FI*310626223
REF*F8*A57B04033
SVC*HC:H0036:GT:UK*-42.58*-42.58**-2
DTM*472*20110102
CAS*CR*141*0*0*42*0*0*22*0*0
CAS*OA*141*0*0
REF*6R*123456
CLP*090909*22*-86.76*-86.76*0*MC*0000000648484848*53
NM1*QC*1*DUCK*DAFFY*W***MI*1245849
NM1*82*2*ABTHSOLUTE HELP*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0004:HF:H9*-86.76*-86.76**-4
DTM*472*20110210
CAS*CR*22*0*0*42*0*0
CAS*OA*22*0*0
REF*6R*090909
LQ*HE*MA92
SE*93*07504123
GE*1*1
IEA*1*004075123
GS*HP*ABCCOM*01017*20110315*1005*1*X*004010X091A1
ST*835*07504123
BPR*H*5.75*C*NON************20110315
TRN*1*A04B001017.07504*1346000128
DTM*405*20110308
N1*PR*ASHTABULA COUNTY ADAMH BD*XX*6457839886
N3*4817 STATE ROAD SUITE 203
N4*ASHTABULA*OH*44004
N1*PE*LAKE AREA RECOVERY CENTER *FI*346608640
N3*2801 C. COURT
N4*ASHTABULA*OH*44004
REF*PQ*1017
LX*1
CLP*444444*1*56.70*56.52*0*MC*0000000655555555*53
NM1*QC*1*FUDD*ELMER*S***MI*1333333
NM1*82*2*WECOVERWY SVCS*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.70*56.52**6
DTM*472*20110205
CAS*CO*42*0.18*0
REF*6R*444444
CLP*999999*4*25.95*0*25.95*13*0000000555555555*11
NM1*QC*1*SAM*YOSEMITE*A***MI*3333333
NM1*82*2*ACME AGENCY*****FI*310626223
REF*F8*H57B10401
SVC*ZZ:M2200:HE*25.95*0**1
DTM*472*20021224
CAS*CR*18*25.95*0
CAS*CO*42*0*0
REF*6R*999999
CLP*888888*4*162.13*0*162.13*MC*0000000456789123*11
NM1*QC*1*SQUAREPANTS*BOB* ***MI*2222222
NM1*82*2*BIKINI AGENCY*****FI*310626223
REF*F8*H57B10401
SVC*ZZ:M151000:F0*162.13*0**1.9
DTM*472*20020920
CAS*CO*29*162.13*0*42*0*0
REF*6R*888888
CLP*111111*2*56.52*18.88*0*13*0000000644444444*53
NM1*QC*1*LEGHORN*FOGHORN*P***MI*7777777
NM1*82*2*CHICKENHAWK SVCS*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.52*18.88**6
DTM*472*20031209
CAS*CO*42*0*0
CAS*OA*23*37.64*0
REF*6R*111111
CLP*121212*4*56.52*0*0*13*0000000646464640*53
NM1*QC*1*EXPLORER*DORA****MI*1717171
NM1*82*2*SWIPER AGENCY*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0005:HF:H9*56.52*0**6
DTM*472*20031202
CAS*CO*42*0*0
CAS*OA*23*57.6*0*23*-1.08*0
REF*6R*121212
CLP*333333*1*74.61*59.69*14.92*13*0000000688888888*55
NM1*QC*1*BEAR*YOGI* ***MI*2222222
NM1*82*2*JELLYSTONE SVCS*****FI*346608640
REF*F8*A76B04054
SVC*ZZ:A0230:HF*74.61*59.69**1
DTM*472*20110203
CAS*PR*2*14.92*0
CAS*CO*42*0*0
REF*6R*333333
CLP*777777*25*136.9*0*0*13*0000000622222222*53
NM1*QC*1*BIRD*TWEETY*M***MI*4444444
NM1*82*2*GRANNY AGENCY*****FI*340716747
REF*F8*A76B03293
SVC*HC:H0015:HF:99:H9*136.9*0**1
DTM*472*20030911
CAS*PI*104*136.72*0
CAS*CO*42*0.18*0
REF*6R*777777
CLP*123456*22*-42.58*-42.58*0*13*0000000657575757*11
NM1*QC*1*SIMPSON*HOMER* ***MI*8787888
NM1*82*2*DOH GROUP*****FI*310626223
REF*F8*A57B04033
SVC*HC:H0036:GT:UK*-42.58*-42.58**-2
DTM*472*20110102
CAS*CR*141*0*0*42*0*0*22*0*0
CAS*OA*141*0*0
REF*6R*123456
CLP*090909*22*-86.76*-86.76*0*MC*0000000648484848*53
NM1*QC*1*DUCK*DAFFY*W***MI*1245849
NM1*82*2*ABTHSOLUTE HELP*****FI*346608640
REF*F8*A76B04054
SVC*HC:H0004:HF:H9*-86.76*-86.76**-4
DTM*472*20110210
CAS*CR*22*0*0*42*0*0
CAS*OA*22*0*0
REF*6R*090909
LQ*HE*MA92
SE*93*07504123
GE*1*1
IEA*1*004075123
EDI
835 Specification:
This X12 Transaction
Set contains the format and establishes the data contents of the Health Care Claim
Payment/Advice Transaction Set (835) for use within the context of the
Electronic Data Interchange (EDI) environment. This transaction set can be used
to make a payment, send an Explanation of Benefits (EOB) remittance advice, or
make a payment and send an EOB remittance advice only from a health insurer to
a health care provider either directly or via a financial institution.
5. Reports and
Acknowledgements
EDI 999 Implementation Acknowledgment:
The EDI 999 transaction set is an Implementation Acknowledgement
document, developed specifically to replace the 997 Functional Acknowledgement document for use in healthcare.
Both the 997 and 999 are used to confirm that a file was received. However, the
999 includes additional information about whether the received transaction had
errors. This includes whether the transaction is in compliance with HIPAA
requirements.
The 999 Acknowledgement may
produce three results:
§ Accepted (A)
§ Rejected (R)
§ Accepted with errors (E)
As a result, the
999 may acknowledge receipt of a transaction, such as a healthcare claim, but
it does not necessarily mean that transaction will be processed. The 999 can
also report on exactly what syntax issues caused the errors in the original
transaction.
The 999 transaction set becomes the standard acknowledgement document for healthcare as of March, 2012, when version 5010 of the HIPAA EDI standards takes effect. The exception to this is the use of a 277 Healthcare Status Notification transaction, used specifically to confirm the receipt of a 276 Health Claim Status Request transaction.
The 999 transaction set becomes the standard acknowledgement document for healthcare as of March, 2012, when version 5010 of the HIPAA EDI standards takes effect. The exception to this is the use of a 277 Healthcare Status Notification transaction, used specifically to confirm the receipt of a 276 Health Claim Status Request transaction.
EDI 999 Format:
ISA*00* *00* *12*4405197800 *01*999999999 *111219*1802*U*00401*000000001*0*T*:
GS*FA*4405197800*999999999*20111219*1802*1*X*004010X098A1
ST*999*0001
AK1*HC*121
AK2*837*987654
AK5*A
AK2*837*987655
AK5*E
AK9*E*2*2*1
SE*8*0001
GE*1*1
IEA*1*000000001
GS*FA*4405197800*999999999*20111219*1802*1*X*004010X098A1
ST*999*0001
AK1*HC*121
AK2*837*987654
AK5*A
AK2*837*987655
AK5*E
AK9*E*2*2*1
SE*8*0001
GE*1*1
IEA*1*000000001
EDI 999 Specification:
This X12 Transaction
Set contains the format and establishes the data contents of the Implementation
Acknowledgment Transaction Set (999) for use within the context of an
Electronic Data Interchange (EDI) environment. The transaction set can be used
to define the control structures for a set of acknowledgments to indicate the
results of the syntactical and relational analysis of the electronically
encoded documents, based upon a full or implemented subset of X12 transaction
sets. The encoded documents are the transaction sets, which are grouped in
functional groups, used in defining transactions for business data interchange.
This standard does not cover the semantic meaning of the information encoded in
the transaction sets.





No comments:
Post a Comment